Comprehensive Guide to Effective Glaucoma Treatment: Latest Options and Tips for Management in 2025
Glaucoma remains one of the leading causes of irreversible blindness worldwide, affecting millions of people each year. Understanding the available treatment options and management strategies is essential for preserving vision and maintaining quality of life. This comprehensive guide explores the latest approaches to glaucoma care, from medications and laser procedures to surgical interventions, helping you make informed decisions about your eye health.
Glaucoma is a group of eye conditions that damage the optic nerve, often due to elevated intraocular pressure. Without proper treatment, this damage can lead to permanent vision loss. Fortunately, modern medicine offers a range of effective treatment options that can slow or halt disease progression when started early and followed consistently.
What Current Research Says About Managing Glaucoma with Medications, Laser and Surgery
Current research emphasizes a multi-faceted approach to glaucoma management. Medications remain the first-line treatment for most patients, with prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors being the most commonly prescribed. Studies show that consistent use of prescribed eye drops can reduce intraocular pressure by 20 to 30 percent, significantly slowing optic nerve damage.
Laser treatments have evolved considerably in recent years. Selective Laser Trabeculoplasty (SLT) has gained popularity as a minimally invasive option that can reduce or eliminate the need for daily eye drops in many patients. Research indicates that SLT can effectively lower eye pressure for several years, with minimal side effects and the possibility of repeat treatments if needed.
Surgical interventions are typically reserved for cases where medications and laser treatments prove insufficient. Traditional trabeculectomy and newer minimally invasive glaucoma surgeries (MIGS) offer different risk-benefit profiles. Recent studies suggest that MIGS procedures provide a safer alternative with faster recovery times, though they may offer slightly less dramatic pressure reduction compared to traditional surgery.
How to Choose the Right Treatment Strategy from Eye Drops to Minimally Invasive Options
Selecting the appropriate treatment strategy depends on several factors including the type and severity of glaucoma, overall health status, lifestyle considerations, and individual response to therapy. Your ophthalmologist will consider these elements when developing a personalized treatment plan.
For newly diagnosed patients with mild to moderate glaucoma, treatment typically begins with prescription eye drops. The choice of medication depends on factors such as efficacy, side effects, dosing frequency, and cost. Some patients may require multiple medications to achieve target pressure levels.
When medications alone prove insufficient or cause intolerable side effects, laser therapy becomes an attractive option. SLT can be performed in an office setting and takes only minutes to complete. Many patients appreciate the reduced burden of daily eye drop administration, though some may still require supplemental medication.
For advanced glaucoma or cases unresponsive to conservative treatments, surgical options should be considered. MIGS procedures such as iStent, Hydrus Microstent, or Xen Gel Stent offer less invasive alternatives to traditional surgery. These devices create new drainage pathways for aqueous humor, reducing intraocular pressure with lower complication rates. Traditional trabeculectomy or tube shunt procedures remain important options for severe cases requiring maximum pressure reduction.
Why Early Detection and Consistent Follow-Up Are Key to Protecting Your Vision
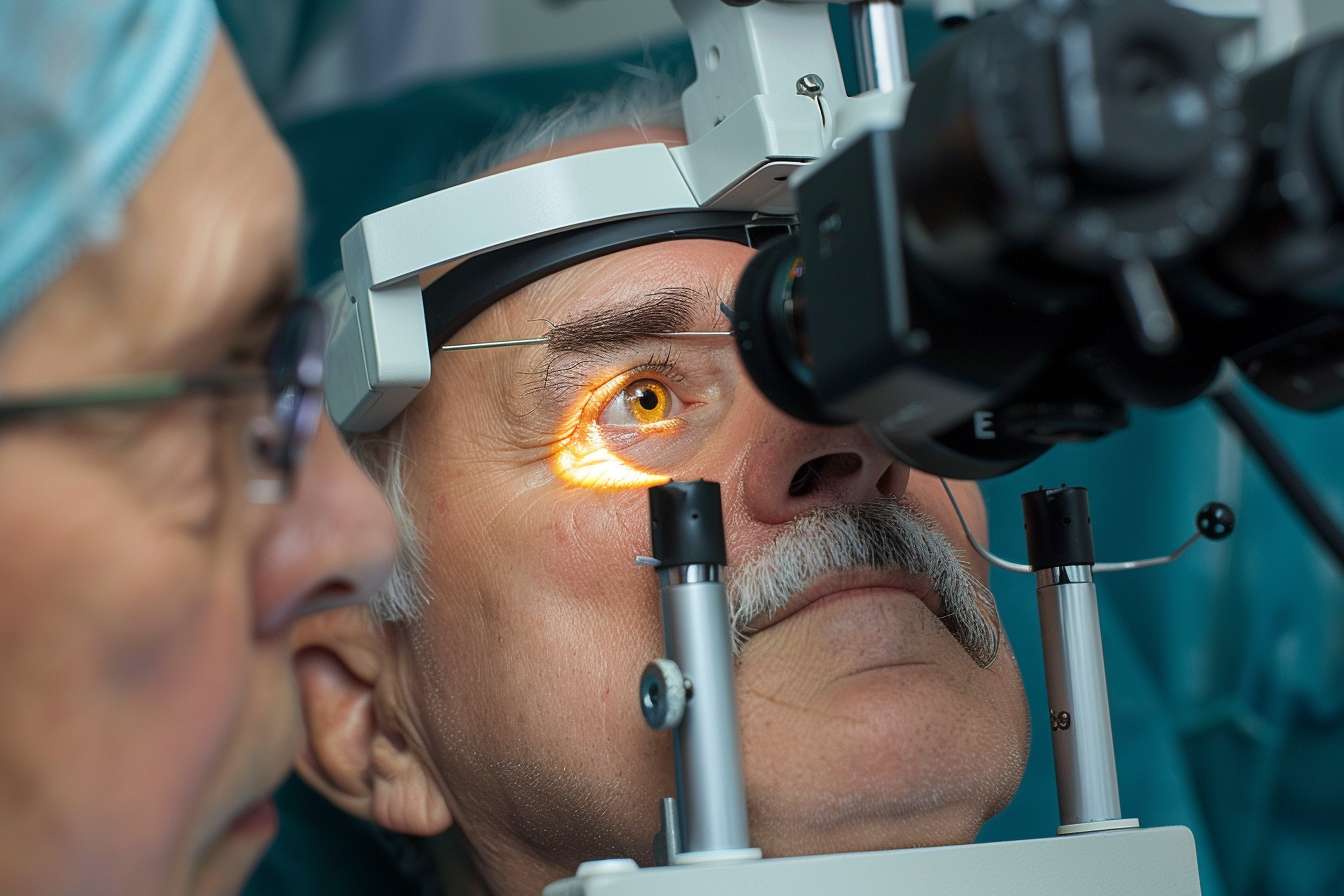
Early detection of glaucoma is crucial because the condition often progresses silently without noticeable symptoms until significant vision loss has occurred. Regular comprehensive eye examinations that include intraocular pressure measurement, optic nerve evaluation, and visual field testing are essential for identifying glaucoma in its early stages.
Once diagnosed, consistent follow-up appointments allow your eye care provider to monitor disease progression and treatment effectiveness. These visits typically occur every three to six months, depending on disease severity and stability. During follow-up examinations, your doctor will assess intraocular pressure, examine the optic nerve for changes, and perform periodic visual field tests to detect any progression.
Adherence to prescribed treatment is equally important. Studies show that many patients struggle with consistent eye drop use, leading to inadequate pressure control and continued optic nerve damage. Setting reminders, establishing routines, and addressing side effects promptly with your doctor can improve medication adherence and treatment outcomes.
Regular monitoring also allows for timely adjustments to your treatment plan. If current therapy proves insufficient, your doctor can add medications, recommend laser treatment, or discuss surgical options before irreversible vision loss occurs. This proactive approach maximizes the chances of preserving functional vision throughout your lifetime.
Understanding the Long-Term Commitment to Glaucoma Management
Glaucoma is a chronic condition requiring lifelong management. Unlike many eye conditions that can be cured, glaucoma treatment focuses on controlling intraocular pressure to prevent further damage. This reality necessitates a long-term commitment to treatment and regular monitoring.
Patients should understand that even successful treatment does not restore vision already lost to glaucoma. The goal is preservation of remaining vision and prevention of future decline. This perspective helps set realistic expectations and emphasizes the importance of early intervention.
Lifestyle modifications can complement medical treatment. Maintaining a healthy diet, exercising regularly, avoiding smoking, and managing systemic conditions like diabetes and hypertension may contribute to better overall eye health. While these measures alone cannot control glaucoma, they support general wellness and may positively influence disease outcomes.
Emotional and psychological support is also important for patients navigating a chronic eye condition. Support groups, educational resources, and open communication with healthcare providers can help patients cope with the challenges of living with glaucoma and maintain motivation for consistent treatment adherence.
Emerging Technologies and Future Directions in Glaucoma Care
The field of glaucoma treatment continues to evolve with promising new technologies on the horizon. Sustained-release drug delivery systems are being developed to eliminate the need for daily eye drops, potentially improving adherence and treatment outcomes. These implants can deliver medication continuously for months, reducing the burden of daily administration.
Advanced imaging technologies allow for earlier detection of glaucoma and more precise monitoring of disease progression. Optical coherence tomography (OCT) provides detailed images of the optic nerve and retinal nerve fiber layer, detecting subtle changes before they become apparent on traditional testing.
Artificial intelligence and machine learning algorithms are being integrated into glaucoma diagnosis and management, helping identify patients at risk and predict disease progression. These tools may enable more personalized treatment approaches and improved outcomes in the future.
Genetic research is uncovering the hereditary factors that contribute to glaucoma development, potentially leading to targeted therapies and better risk assessment for family members of affected individuals. As our understanding of glaucoma genetics grows, prevention strategies may become more sophisticated and effective.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




